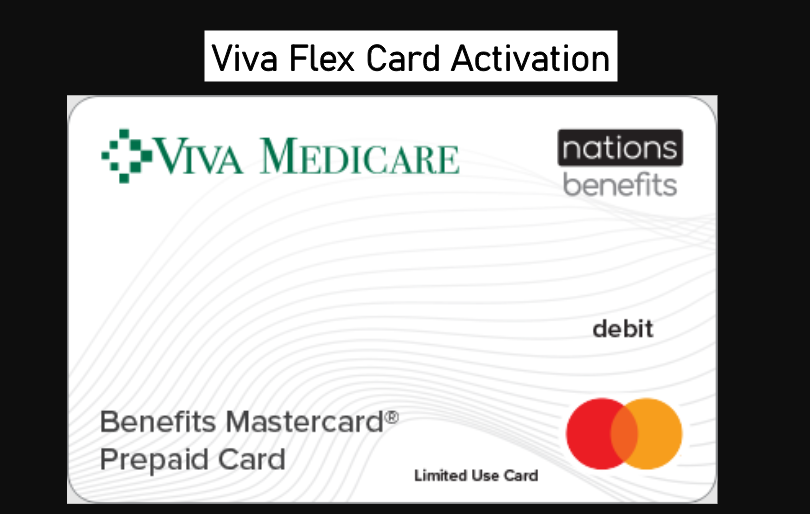
viva.nations benefits.com Login Activate Flex Card
Viva.nations Benefits Login: How to Activate Your Flex Card 2023
Are you having trouble logging into your benefits page or want to receive a hard copy of your plan materials? Look no further! Contact Viva Health Customer Service for assistance at (800) 294-7780 (toll-free) or (205) 558-7474 (local). Representatives are available from 8 am to 5 pm, Monday to Friday.
Sample Viva Health ID Card
To access your plan materials, you’ll need your Family ID number and ID Suffix number. You can find these numbers on your Viva Health ID card (highlighted in red). For example, if your numbers are “0123456700,” that’s what you’ll enter.
How to Login and Activate Your Card on Viva.nations Benefits
Once you have received and activated your card, you can start using it online through the MyBenefits portal and app or in person at a participating retail location near you. Here are the steps to activate your card:
- Visit viva.nationsbenefits.com or call 877-209-5189 (TTY: 711)
- Enter the 16-digit card number and expiration date of your Benefits Mastercard® Prepaid Card.
- Enter your 12-digit Member ID (contains 2 letters and 10 numbers).
- Enter your Date of Birth and Last Name as provided to your health plan during enrollment.
- Click on the Activate Card button.
Ordering OTC Products
Ordering OTC products is easy and can be done online, by phone, or mail. Here’s how:
Online: Visit NationsBenefits.com/Viva. Phone: Call 877-209-5189 (TTY: 711). Mail: Complete and mail an order form to NationsOTC.
If you need assistance with your order, call 877-209-5189 (TTY: 711). Member Experience Advisors are available from 8 am to 8 pm until December 31, 2021. Beginning January 1, 2022, NationsOTC will be open 24/7/365.
Determining Your Primary Health Plan
Some members have coverage under multiple private plans, such as individual, student, and employer-based coverage. To determine which plan is primary, follow these rules in order:
- The plan with no coordination of benefits provision or non-duplication coverage exclusion is always primary.
- The plan that covers you as a subscriber (policyholder) is primary.
- The plan of the parent whose birthday comes first in the calendar year is primary for dependent children coverage.
- If none of the above rules apply, the plan that has covered you the longest is primary.
How to Access Your Plan Materials
Online Access through MyBenefits Portal and App
To access your plan materials online, follow these steps:
- Visit viva.nationsbenefits.com or call 877-209-5189 (TTY: 711)
- Enter your 16 digit card number and expiration date of your Benefits Mastercard® Prepaid Card
- Enter your 12-digit member ID (2 letters and 10 numbers)
- Enter your Date of Birth and Last Name provided to your health plan during enrollment
- Click on the Activate Card button to activate your card
Hard Copy Request
To request a hard copy of your plan materials, contact Viva Health Customer Service at:
- Toll-free: (800) 294-7780
- Local: (205) 558-7474 Representatives are available Monday through Friday between the hours of 8am and 5pm.
Ordering Over-the-Counter (OTC) Products
Online Ordering
Visit NationsBenefits.com/Viva to place an online order.
Phone Ordering
Call 877-209-5189 (TTY: 711) to place a phone order.
Mail Ordering
To place a mail order, complete and send an order form to NationsOTC.
For assistance with your order, call 877-209-5189 (TTY: 711). Member Experience Advisors are available 8am – 8pm until December 31st, 2021. Beginning January 1st, 2022, NationsOTC will be open 24 hours per day, 7 days per week, 365 days per year.
Plan Coordination of Benefits
If you have coverage under multiple private plans, such as individual, student, and employer-based coverage, it can be confusing to know which plan is primary. Here are four rules to determine the priority order of benefits:
- The plan with no coordination of benefits provision or non-duplication coverage exclusion is always primary. All Viva Health plans have a coordination of benefits provision.
- The plan that covers a member as a subscriber (policyholder) is primary.
- The plan of the parent whose birthday comes first in the calendar year is primary with respect to coverage for enrolled dependent children. There are additional rules for divorced or separated parents. See your Certificate of Coverage (COC) or call Customer Service for more information.
- If none of the rules above determine the order of benefits, the plan that has covered you the longest is primary.
Features of the NationsOTC Solution
- CMS-compliant and fully customizable program
- 24/7/365 live customer service
- Comprehensive product formulary, including healthy foods and connectivity devices
- Competitive product pricing
- Five national distribution centers
- Nationwide 2-day delivery, at no additional cost
Member Portal
The Member Portal provides robust search options with the ability to filter, sort, and search by category, pricing, wallet, and more. The portal also offers:
- Product recommendations based on individual needs
- Expandable product detail pages with 360-degree images
- Benefit tracking to see available dollars to spend on plan-approved products
- Order tracking with carrier details and frequent status updates
To access the Member Portal, visit members.nationsbenefits.com/aetna and activate your card. After completing your profile registration, you will be prompted to activate your card if you have the OTC Card in your possession.
People Read Also:
- bluekc nationsbenefits com log in
- optimum nationsbenefits com login
- freedom.nationsbenefits.com Activate Card link
- Central Health Plan nationsbenefits com Activate Card






One Comment